Virginia A. Caine, M.D., to propose safe syringe exchange to City-County Council
INDIANAPOLIS – With a backdrop of supportive leaders representing civic, religious, health care and public safety organizations, Marion County Public Health Department director Virginia A. Caine, M.D., today proposed the county’s first-ever syringe exchange program to combat the alarming increase in hepatitis C cases and to prevent a potential surge in HIV cases.
Caine began the day with a briefing session to public health organizations in Marion County, including those that work on the many issues impacting individuals suffering from drug addiction. She provided detailed statistics, which show a 1,000 percent increase in the number of hepatitis C cases from 2013 to 2017, a majority of which have been attributed to injection drug use.
Given the level of increase – and seeking to prevent an HIV outbreak similar to what Scott County, Indiana experienced in 2015 – Caine declared a public health epidemic for Marion County, the first step required by Indiana law for a county to implement a syringe exchange program. Once an epidemic is declared, the second requirement is approval by the City-County Council.
“After careful study and analysis, I am declaring an epidemic that is putting Indianapolis in a public health emergency for hepatitis C in Marion County,” Caine said. “The proposed syringe exchange program is medically necessary and will save lives by reducing the transmission of hepatitis C and HIV. Both are growing national problems brought on by the widespread increase in opioid addiction.”
City-County Council President Vop Osili joined the announcement and expressed his support for the syringe exchange program. He indicated the program would be introduced for consideration at the council’s next meeting on May 21.
“I strongly support moving forward with a syringe exchange program as it will improve public health in Indianapolis and Marion County while also saving taxpayers money by greatly reducing the burdensome health care costs related to injection drug use and infectious disease,” said Osili.
Osili stressed that the program will require no additional public investment, with conservative estimates showing a potential annual savings for taxpayers and health care providers of $193 million in HIV treatment costs alone.
Caine highlighted several data points signifying the troubling surge in both hepatitis C and HIV in Marion County:
· The rate of reported acute hepatitis C infection in Marion County rose from 0.6 to 7.6 per 100,000 population between 2013 and 2017.
· That rate is likely understated. The Centers for Disease Control and Prevention (CDC) estimates that true number of acute hepatitis C cases are nearly 14 times what is reported, which translates to approximately 1,000 new cases in Marion County in 2017 alone.
· In at least 86 percent of the new cases in 2017, patients reported injecting drugs within the last six months, and at least 58 percent reported sharing drugs and paraphernalia.
· The CDC estimates a prevalence between 9,200 and 11,400 cases of chronic hepatitis C for a population of Marion County’s size; however, more than 21,000 county residents with chronic hepatitis C have been reported since 1990.
· HIV cases have also spiked. Newly reported HIV cases were decreasing steadily from 2011 to 2015 but in 2017, the rate per 100,000 was 25.3, up from 20.0 in 2015.
Caine said the proposed program would ensure injection drug users have access to clean needles to prevent infections, keep used needles off the streets and connect individuals with needed health services.
Initially, the program would operate as a mobile unit. Sites would be based on overdose deaths by location, residences of decedents, Indianapolis EMS use of Narcan, and recommendations by the Indianapolis Metropolitan Police Department.
Support services vital to the program would include:
· HIV and hepatitis C rapid screening
· Safer drug use practices
· Referral for substance use disorder and mental health treatment
· Wound care education
· Immunizations
· Referral to primary care
· Access to health insurance coverage
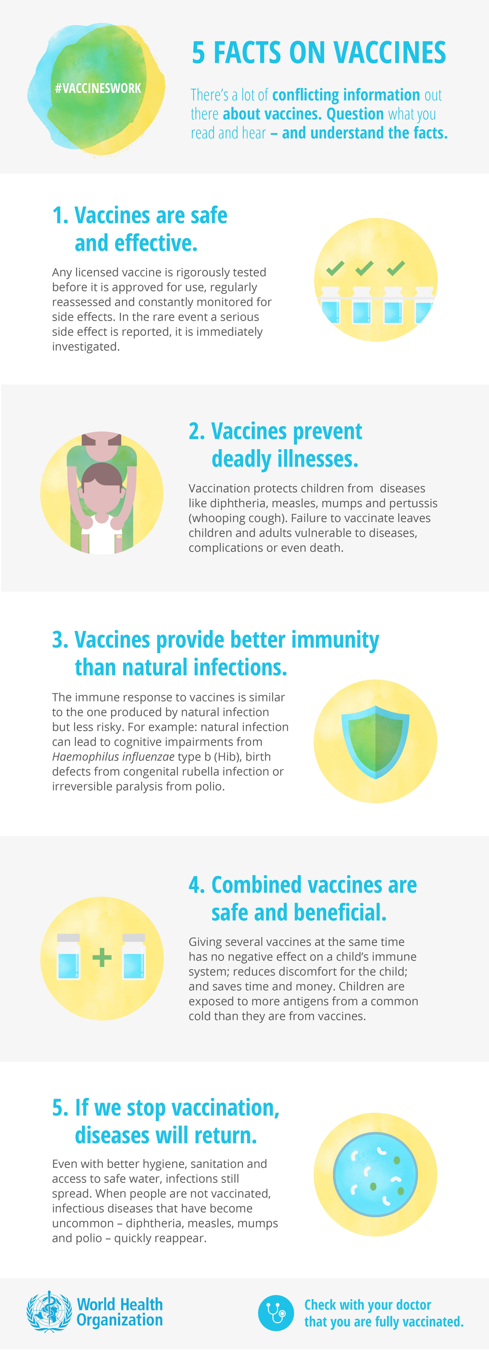
Studies show that participants in a syringe exchange program are five times more likely to enter drug treatment than injection drug users who do not participate in the program.
Caine also highlighted national statistics and the successes of other counties in Indiana that have implemented a similar program. She cited CDC findings that syringe exchange programs:
· Curtail drug use
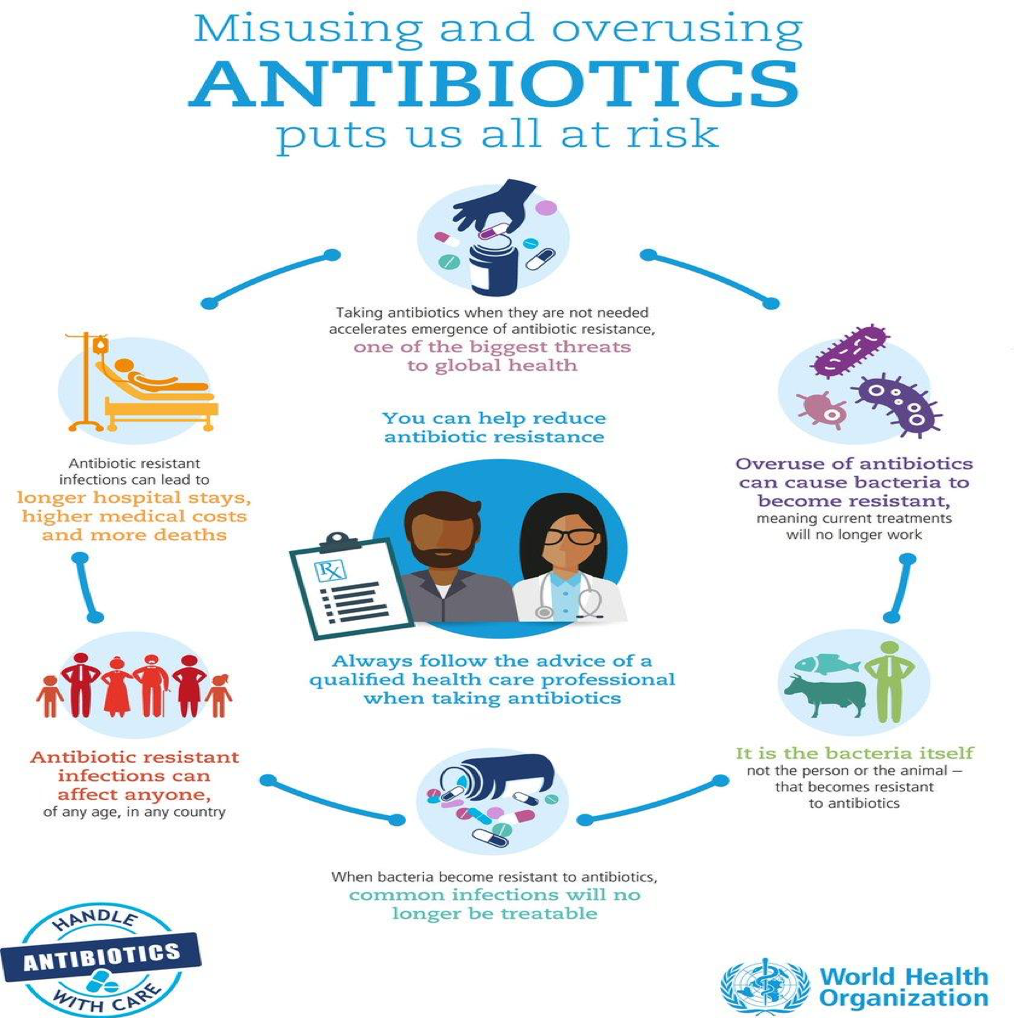
· Reduce needlestick injuries among first responders
· Decrease overdose deaths
For more information, visit marionhealth.org/SafeSyringe.
What are Marion County health care and health education leaders saying about this health emergency and safe syringe program?
Krista Brucker, M.D., Medical Director of Project POINT and an Emergency Medicine Physician at Eskenazi Health
“At first glance, a syringe service (needle exchange) program might seem counter intuitive, but I'm an ER doctor on the front lines of this epidemic and I can tell you that we need all the tools we can muster to help stem the tide of needless death and disease. Syringe service programs have decades of evidence showing that people who use them, use less drugs, use more safely, are more likely to get into medical care and less likely to transmit diseases like HIV and hepatitis C. Beyond the evidence, I can assure you that when our patients are in the depths of active addiction beyond where they can hear or feel the love and support of family, friends or others who are trying to help, a syringe service program may be the only way to reach them. It is the only place that feels safe and non-judgmental, where they can begin to build the trusting relationships that might help them take those first painful steps into recovery.” – Krista Brucker, M.D., Medical Director of Project POINT and an Emergency Medicine Physician at Eskenazi Health
Naga Chalasani, MD, David W. Crabb Professor and Associate Dean for Clinical Research, Director, Division of Gastroenterology and Hepatology, Indiana University School of Medicine
“As a physician and researcher who specializes in liver diseases, I support the establishment of a needle exchange program in Marion County. Once acquired, both hepatitis C and HIV can become lifelong diseases with major consequences not just for suffering individuals and their families, but for tax payers as well. Needle exchange programs have repeatedly been shown to be effective in reducing the rates of hepatitis C and HIV infections.” – Naga Chalasani, MD, David W. Crabb Professor and Associate Dean for Clinical Research, Director, Division of Gastroenterology and Hepatology, Indiana University School of Medicine
Joan Duwve, MD, MPH, Associate Professor, Associate Dean of Public Health Practice, IU Richard M Fairbanks School of Public Health at IUPUI
“The IU Richard M. Fairbanks School of Public Health at IUPUI is committed to improving the health of all Hoosiers through evidence-based practices. We continue to work with community partners statewide to prevent opioid misuse and respond to the epidemic of opioid overdose and death. Syringe services programs have been proven to reduce the spread of hepatitis C
and HIV in communities, and do not increase drug use. They also reduce overdoses and death by offering their clients naloxone and referral to addiction treatment programs. We support the Marion county decision to open a syringe services program to promote the health of its residents by addressing the worsening epidemics of hepatitis C and drug overdose death in the community." — Joan Duwve, MD, MPH, Associate Professor, Associate Dean of Public Health Practice, IU Richard M Fairbanks School of Public Health at IUPUI
Richard K. Freeman, MD, MBA, Chief Medical Officer, St. Vincent Indiana
“St. Vincent Indiana is committed to delivering compassionate, personalized care to all, with special attention to those who are most vulnerable. We recognize the public health challenge before us and the opportunity through outreach to encourage individuals suffering from the illness of addiction to enter treatment.” – Richard K. Freeman, MD, MBA, Chief Medical Officer, St. Vincent Indiana
Karen Hardin DNP, RN, NE-BC, CNE, Director Workforce Development, Coordinator of Faith Community Nursing Program, Assistant Professor, Marian University
“As a nurse, you are called to this profession because of a desire to do something important. You want to make a difference in the lives of others. You want a career that taps into all that you are. Our country and county are facing a health crisis. We want to do something important to make a difference and to tap into all in what we are. We are proud to stand with Marion County Public Health Department.” – Karen Hardin DNP, RN, NE-BC, CNE, Director Workforce Development, Coordinator of Faith Community Nursing Program, Assistant Professor, Marian University
Lisa E. Harris, M.D., CEO, Eskenazi Health
“At Eskenazi Health, we follow a patient-focused model of care that encourages participation with an emphasis on prevention. Implementing Safe Syringe is a medically necessary step that has been proven to immediately reduce the transmission of hepatitis C and HIV. It will also greatly increase the likelihood of individuals entering treatment programs for opioid addiction. This program will save money and more importantly will save lives.” – Lisa E. Harris, M.D., CEO, Eskenazi Health
Leslie A. Hulvershorn, MD, Assistant Professor of Psychiatry, Indiana University School of Medicine
“I applaud the decision to establish a needle exchange in Marion County. In addition to reducing the spread of hepatitis and HIV, needle exchange programs also connect individuals with substance use disorders to important treatment resources that can help them work toward recovery from injection drug use. We know that people who engage with treatment providers are many times more likely to recover from substance use disorders.” – Leslie A. Hulvershorn, MD, Assistant Professor of Psychiatry, Indiana University School of Medicine
Kathleen Lee, Ed.D., Chancellor, Ivy Tech Community College Indianapolis
“As the State of Indiana’s Community College system we believe it is necessary to support our local communities in a variety of ways. One such way is to promote the public health of those communities. Ivy Tech supports Dr. Caine and her staff as they implement a needle exchange program to combat the transmission of Hepatitis C. This program, although not a treatment for drug use or Hepatitis C has been proven to reduce the prevalence of new infections and increases testing and education. We stand ready to assist Dr. Caine in educational efforts related to a needle exchange program.” – Kathleen Lee, Ed.D., Chancellor, Ivy Tech Community College Indianapolis
Ryan D. Nagy, MD, President, Adult Academic Health Center, Indiana University Health
“From a medical perspective, we know that syringe exchange programs are proven to save lives and reduce the spread of disease. They also can serve as a first step toward helping people with substance abuse disease. The Safe Syringe program is a medically necessary effort to address this growing crisis in our county." – Ryan D. Nagy, MD, President, Adult Academic Health Center, Indiana University Health
Luke Nelligan, D.O., Interim Associate Dean for Clinical Affairs, Marian University
“The whole person approach to healing is what osteopathy is all about, so the 2013 opening of an osteopathic medical school was the obvious path for a Franciscan institution already dedicated to the education and nurturing of mind, body, and spirit. It is our whole person approach, which brings us to support efforts to reduce this health emergency and to support efforts which will reduce the spread of Hepatitis C and bring more people into treatment and recovery.” – Luke Nelligan, D.O., Interim Associate Dean for Clinical Affairs, Marian University
Robin P. Newhouse, PhD, RN, NEA-BC, FAAN Dean and Distinguished Professor, IU School of Nursing
“The IU School of Nursing has been empowering leaders for more than 100 years. Many of our faculty conduct research to study a wide variety of healthcare issues, including quality of life in chronic illness such as Hepatitis C. We are proud to stand with Dr. Caine and Marion County Public Health Department as they take the medically necessary steps to address this health emergency and reduce the number of individuals at risk of Hepatitis C infection and bring more people into recovery.” – Robin P. Newhouse, PhD, RN, NEA-BC, FAAN Dean and Distinguished Professor, IU School of Nursing
Charles M. Miramonti, M.D., Chief of Indianapolis Emergency Medical Services (IEMS), Chief of Care Integration and an Emergency Medicine Physician at Eskenazi Health, Associate Professor of Clinical Emergency Medicine at the Indiana University School of Medicine
“Many people in the community don’t realize how often overdoses actually occur. On average, IEMS dispatches 15 overdose runs every day at hotels, gas stations even in parked cars. A syringe exchange program is what our community needs right now to combat and reduce the
impending hepatitis crisis. This program will make our first responders and community safer.” – Charles M. Miramonti, M.D., Chief of Indianapolis Emergency Medical Services (IEMS), Chief of Care Integration and an Emergency Medicine Physician at Eskenazi Health, Associate Professor of Clinical Emergency Medicine at the Indiana University School of Medicine
Dr. Robin Ledyard, Community Health Network Chief Medical Officer
“We know people who enter syringe exchange programs are more likely to get into treatment. Addiction is a disease, and if we can help at any entry point to get someone treatment, then we are on the right path.” – Dr. Robin Ledyard, Community Health Network Chief Medical Officer
Mary Ian McAteer, MD, President, Indianapolis Medical Society
“The future of our country depends on the health and wellbeing of our children. It is imperative that we physicians advocate for strong policies that enable physicians, patients, families and communities to work together to create the healthiest environments for our children. As physicians, we stand shoulder to shoulder with Dr. Caine as she implements a medically necessary and evidence-based program to address this medical emergency and encourage more people to take a path of recovery, restoring families and providing a safer and healthier community for our children and all citizens.” – Mary Ian McAteer, MD, President, Indianapolis Medical Society
Bree A. Weaver, MD, Assistant Professor of Clinical Medicine and Clinical Pediatrics, Indiana University School of Medicine
“As we have seen before in Indiana, an increase in cases of hepatitis C can also be a precursor to a rise in HIV infections. As an infectious disease specialist, addressing HIV and hepatitis C and preventing new infections are my highest priorities, and a syringe exchange is a major step toward this objective.” – Bree A. Weaver, MD, Assistant Professor of Clinical Medicine and Clinical Pediatrics, Indiana University School of Medicine
Emily Zarse, M.D., Chief of Addiction Services for Eskenazi Health Midtown Community Mental Health
“Opioid addiction is increasing in our nation and community. It is an illness that affects people of all ages and from all walks of life. Individuals participating in Safe Syringe will be dramatically less likely to contract or spread Hepatitis C or HIV and five times more likely to seek treatment for their illness of addiction.” – Emily Zarse, M.D., Chief of Addiction Services for Esk